Blood biomarkers for Alzheimer’s disease: Reliable change and impacts of renal and blood–brain barrier function
- Post by: Alper Idrisoglu
- 8 September, 2025
- No Comment
Abstract
Introduction
Blood-based biomarkers for Alzheimer’s disease (AD) have the potential to improve diagnostic accessibility, but their clinical interpretation requires understanding of variability and biological influences.
Methods
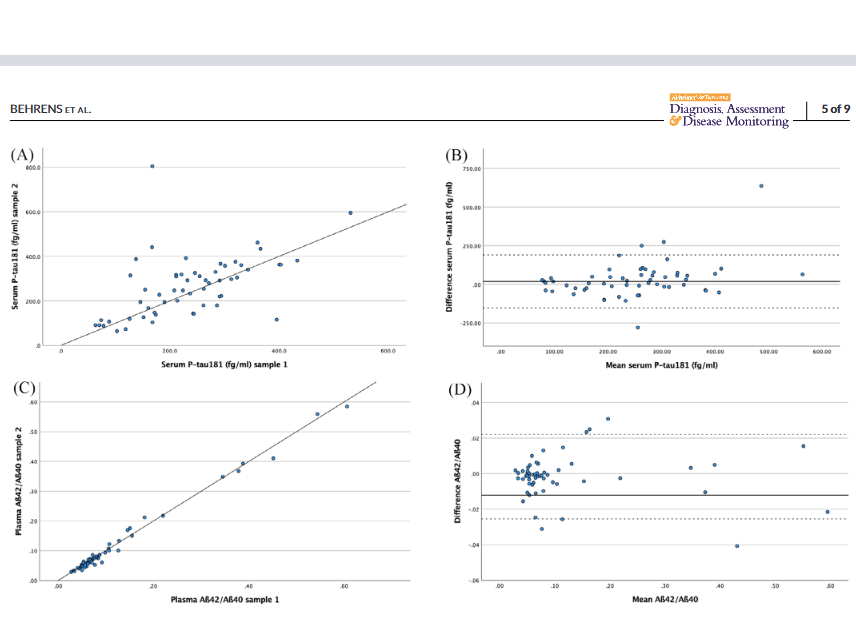
We repeatedly sampled blood from 57 adults referred for lumbar puncture as part of a cognitive evaluation at a memory clinic. We measured serum phosphorylated- tau-181 (s-p-tau181) and plasma amyloid beta (Aβ)42/40 ratio (p-Aβ42/Aβ40) and evaluated the impact of renal and blood–brain barrier (BBB) function.
Results
Test–retest analysis revealed large variability of s-p-tau181 and small for p-Aβ42/Aβ40. Markers of renal function and BBB integrity significantly influenced s-p-tau181 levels, whereas p-Aβ42/Aβ40 was not affected.
Discussion
This study emphasizes the need for caution when interpreting longitudinal changes in s-p-tau181. Inter-individual variability is to a large degree due to susceptibility to biological influences where a novel association with integrity of BBB function were identified. These results have implications for the clinical application of blood-based biomarkers in AD diagnostics and monitoring.
Highlights
- Blood phosphorylated- tau-181 (p-tau181) shows high test–retest variability in memory clinic patients.
- Blood amyloid beta (Aβ)42/Aβ40 ratio is stable but has poor diagnostic accuracy.
- Renal function and blood–brain barrier (BBB) integrity affect blood p-tau181 levels.
- Caution is needed when interpreting longitudinal changes in blood p-tau181.
- Renal and BBB disorders should be considered when assessing blood p-tau181.
Keywords
Alzheimer’s disease, biomarker validation, blood biomarkers, clinical interpretation, dementia diagnosis, neurodegenerative disease, test–retest variability
DOI: https://doi.org/10.1002/dad2.70181
